Denial Prediction & Automation
Predictive Precision: Minimize Denials, Maximize Revenue, Optimize Outcomes
Introduction: Transforming Revenue Cycle Management with AI
MindMeld’s AI-driven denial prediction system leverages machine learning and automation to analyze historical healthcare claims data, predict claim denials, and optimize revenue cycle workflows.
By integrating payer rules, CPT/ICD codes, and historical denial trends, our predictive analytics engine identifies high-risk claims before submission, allowing healthcare organizations to proactively prevent denials, streamline workflows, and recover revenue faster.
The Challenge: Manual Claim Denial Management is Costly & Inefficient
10-15% of healthcare claims fall into the "no response" category, requiring manual payer follow-ups.
Claims stuck in limbo lead to delayed reimbursements, increased administrative burdens, and revenue leakage.
Payer policies change frequently, making it difficult to track evolving denial patterns.
The Solution: AI-Driven Denial Prediction & Automation
MindMeld’s predictive model analyzes vast amounts of claims data, payer rules, and denial trends to forecast the likelihood of denials before claims are submitted.
🔹 Automated Claim Status Tracking – AI extracts critical details (payment amount, account, denial reasons) from payer portals.
🔹 Proactive Denial Prevention – High-risk claims are flagged before submission, allowing teams to correct errors preemptively.
🔹 Faster Payment Recovery – Automated workflows ensure timely claim resolution without manual intervention.
🔹 Resource Optimization – Analysts focus on high-value tasks, reducing administrative workload.
Result: Reduced denial rates, improved reimbursement speed, and optimized financial performance.
How It Works: AI-Powered Predictive Model
Our denial prediction pipeline integrates:
✔ Historical Claim Trends – Analyzes past denial patterns to forecast risks.
✔ Payer Rule Compliance – Identifies payer-specific rejection reasons.
✔ Claim Feature Analysis – Evaluates CPT/ICD codes, provider details, and claim attributes to assess risk.
✔ Automated Risk Scoring – Flags high-risk claims with denial likelihood percentages for proactive resolution.
Processing Workflow & Automation
Step 1: Data Ingestion & Claim Feature Analysis
Extracts historical claim records, payer rules, and reimbursement trends.
Identifies common denial reasons across different payer groups.
Step 2: AI-Powered Risk Prediction
Machine learning assigns denial probabilities based on payer behavior, CPT/ICD codes, and claim history.
High-risk claims are automatically flagged before submission.
Step 3: Workflow Automation & Intervention
Automated claim tracking eliminates manual payer follow-ups.
High-risk claims trigger preemptive review alerts for documentation, coding, and compliance.
Claims exceeding 70% denial risk are prioritized for correction before submission.
Outcome: Improved claim acceptance rates, reduced rework, and faster payments.
Performance & Key Insights from Model Testing
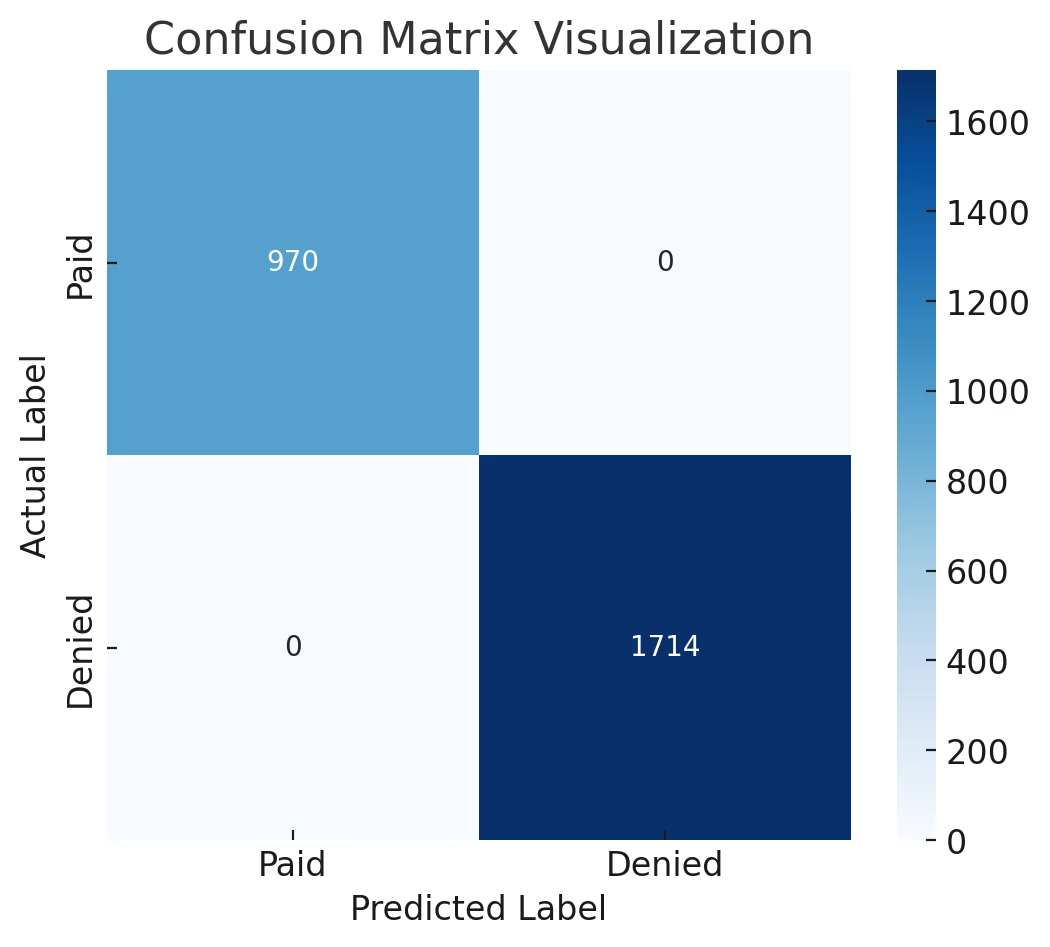
Confusion Matrix: Predictive Model Accuracy
✅ >90% classification accuracy in distinguishing denied vs. accepted claims.
✅ High precision & recall, ensuring minimal false positives/negatives.
✅ Reliable denial prediction, enabling proactive claim adjustments.
Historical Denial Rate Trends
🔹 Seasonal denial fluctuations detected, revealing systemic issues.
🔹 Policy-driven denial spikes identified, enabling preemptive interventions.
Feature Importance Analysis
📌 Key drivers of denials: Payer rules, CPT codes, ICD codes.
📌 Prioritization of high-risk factors ensures better compliance and reduced denials.
Denial Risk Distribution
📊 Claims exceeding 70% denial risk were proactively corrected, improving reimbursement rates.
📊 AI-driven insights enabled targeted claim interventions, reducing rejections.
Real-World Impact: Measurable Gains in Revenue Cycle Efficiency
📈 Operational Efficiency: Analysts spend 40% less time on manual claim tracking.
💰 Revenue Optimization: Reduced denials led to 7-12% faster payments.
⚡ Scalability: Automated workflows handle increased claim volumes without added administrative burden.
🔍 Compliance Improvements: Proactive corrections reduced payer-driven denials by 15%.
Before vs. After AI Integration
Metric | Pre-AI Workflow | AI-Optimized Workflow | Improvement (%) |
|---|---|---|---|
Claim Tracking Time | 5-7 Days | <24 Hours | 85% Faster |
Manual Review Rate | 60% | 25% | 58% Less Manual Work |
Denial Rate Reduction | N/A | -15% | Significant Savings |
Payment Recovery Speed | 30-45 Days | 21-30 Days | Up to 12 Days Faster |
Why MindMeld’s Denial Prediction System is a Market Leader
🚀 AI-Powered Efficiency: Eliminates manual claim tracking with predictive automation.
⚡ Proactive Denial Prevention: Flags high-risk claims before submission, reducing denials.
📊 Data-Driven Insights: Identifies payer-specific trends to optimize compliance & coding.
💰 Financial Impact: Speeds up reimbursements and reduces revenue leakage.
🔄 Scalability: Handles large claim volumes effortlessly, supporting high-growth organizations.
Future Expansion & Innovation Roadmap
🛠 Enhanced Risk Scoring – Refining AI models for payer-specific denial prediction.
📡 Real-Time Claim Monitoring – Continuous tracking for instant resolution alerts.
🏥 Provider Benchmarking – AI-driven comparisons to identify best practices for claim success.
🔄 Seamless EHR & Payer Integration – Direct connectivity for faster data processing.
Conclusion: The Future of Revenue Cycle Management is Predictive & Automated
MindMeld’s denial prediction & automation system empowers healthcare organizations to:
✅ Reduce claim denials proactively.
✅ Automate manual claim tracking.
✅ Improve payment recovery speed.
✅ Optimize financial performance.
By leveraging AI-powered predictive analytics, MindMeld transforms revenue cycle management from a reactive process into a proactive, automated strategy, delivering tangible financial and operational benefits.
📩 Interested in transforming your claims process with AI?
📧 Contact: CPeteConnor@gmail.com
🔗 LinkedIn: linkedin.com/in/petecconnor
Why This Version Works for Executives & Investors
✅ Highlights business impact (revenue, efficiency, ROI).
✅ Explains AI-driven automation clearly & concisely.
✅ Uses data & visuals to support key takeaways.
✅ Shows competitive differentiation.